
I Got COVID 9 Months Ago and Still Have Symptoms (Newsweek)
Dec 16, 2020'I Got COVID 9 Months Ago and Still Have Symptoms'
Dr. Melissa Geraghty
On 12/2/20 at 5:51 AM EST
At the beginning of 2020, when COVID-19 was still only in the peripheries of our awareness, I was recovering from neurosurgery. I have a rare neurological disease, tethered cord syndrome, and in October 2019 I had been through an invasive operation to detach my spinal cord from where it had connected to the surrounding tissue. Just 10 days later, I had another surgery to repair a CSF (cerebrospinal fluid) leak.
Severe pain and complex symptoms have been part of my life since as long as I can remember. Even after the neurosurgery, I was in physical therapy, using my recumbent bike daily, and receiving weekly ketamine infusions for hyperalgesia. I was trying desperately to find my new chronic illness baseline. Despite all this, I still saw patients in my role as a psychologist four to five days a week, often working until 8pm.
Then, around 250 days ago, I was diagnosed with COVID-19.
In early March, I was the first person that myself or my physicians knew with COVID-19. I was leading the way with a diagnosis of a disease people didn't know much about at the time. Unfortunately, a familiar role for me.
Later in March as my conditions worsened, I had my first emergency room (ER) visit. I was told I likely had a sinus infection and anxiety. I remember explaining that I wasn't experiencing heightened anxiety, but at that time they would not test me for COVID and discharged me. My physician sent me back to the ER seven days later with worsening symptoms—I was finally tested.
Since then, I have exhibited an exhausting number of symptoms. At one stage I spiked with fever multiple times a day for more than 80 days, I have experienced lung pain and pressure, extreme mental and physical fatigue, labored breathing, full body aches, brain fog, shortness of breath from standing or walking, increased headaches and migraine attacks, diarrhea, bloating, stomach gurgling, tinnitus, hot and cold sweats, loss of smell and a dry cough. That isn't even the full list. Now consider that I am still experiencing a huge range of these symptoms nearly nine months later. As a long-haul COVID-19 sufferer, one of many thousands in the U.S., it's been hard not to feel that my body has been kicking me while I'm already down.
When I unknowingly became ill with COVID-19—likely from an asymptomatic person—I had already implemented social distancing at my office and was careful to wipe down and disinfect all surfaces after each patient. Then, we weren't yet wearing masks, as this was well before mask mandates and more detailed information about the virus was available. As a clinical health psychologist in Illinois who sees immunocompromised patients, I'm so thankful that I took it upon myself to take these precautions—and I am not aware of any of my patients contracting COVID-19 from me.
One night early on, I felt like I was having a heart attack. My blood pressure dropped and I experienced a surreal, out of body feeling. I didn't call 911, mainly because I had been to the ER numerous times by this point—I felt like there was little they would be able to do to help me. I was also concerned that I may be viewed as a drama queen. Patients with chronic pain can often be stereotyped, especially when they present with symptoms that are unusual. It then took a week for me to get an echocardiogram and I had to travel an hour away for it since local facilities and hospitals wouldn't admit a COVID-positive patients for the procedure. I understand the precaution, but it can make you feel helpless in a situation where you are relying on others for help.
Were we not in the middle of a pandemic, it's likely that I would have been hospitalized on that first ER visit. However, hospital beds were reserved for the sickest of the sick. I was in an odd, and frightening, position of being too sick to be at home, but not sick enough to be hospitalized. At home I would wonder: Will I get worse and then be admitted only to find out it's too late? Will I die at home? What damage has already been wrought on my body from this virus?
I had to take multiple days off from telehealth with patients in the early weeks of my COVID-19 diagnosis, so I'm fortunate to have such amazing and understanding patients. Many of them saw me sweating and looking half-dead with an oxygen tank beside me. I know it was hard for my patients to see me like that, but we would have open conversations about my illness. Often, they were concerned that I was still working; I would tell them how I felt a huge part of being able to make it through each day was the time spent working with them.
But an hour long session could feel like an eternity during the times when my insides felt like they were screaming, and sometimes that is still the case. I am used to being able to focus when experiencing intense pain and parallel symptoms from my neurological disorder, but the ongoing effects of COVID-19 have added a completely different dimension. I wondered if I was pushing myself beyond my limits, or whether continuing to work was helping me survive mentally.
As an independent contractor who doesn't get paid for holiday or sick leave, I felt that I had to keep working. I have more medical bills than most and graduate student loans to pay off. There was also the concern around the continuity of care for my patients. Many had refused to see another therapist while I was taking sick leave for my neurosurgery. I also couldn't easily transfer them as I am highly specialized and typically work with complex individuals.
Another factor for me is the fear that if I did take an extended period away from work, my mental health would suffer so greatly that I would never be able to return to work as a psychologist. It is an utterly terrifying thought.
In the early stages of my COVID illness, I experienced a huge number of flashbacks from past medical experiences that were similar. At first I didn't even realize I was experiencing medical PTSD until the director of the private practice I work at gently pointed it out to me. Psychologists are often very aware of secondary trauma and since March it has felt like my current symptoms and the trauma from my neurological disease have been existing in a kind of horrifying parallel.

Dr. Melissa Geraghty in the emergency room following her neurosurgery in October 2019. Dr. Melissa Geraghty
COVID-19 continues to wreak havoc on my body, nine months after I was first diagnosed. My primary care physician (PCP) remains concerned about my ongoing symptoms and we have discussed my long-haul COVID at length. Last week I took another round of steroids to no avail and I will soon be getting another Echocardiogram and a Pulmonary Function Test. At the moment, I'm just trying to breathe and not pass out during sessions. I am doing this during six consecutive hours working with patients who are all experiencing their own trauma.
As COVID has lingered with me, and surged again across the globe, some patients have discussed going out with friends as I sit on the other side of the telehealth screen, still struggling with breathing. They saw me at my worst. But I don't have it in me to discourage their reckless behavior; they know the risks because we've discussed them multiple times. Instead, I lean in and provide compassion and empathy. I think if I cease to be able to offer that, I would know it was my cue to leave the profession.
I'm now only working three days a week, with no late nights, and I go to bed before 7pm most nights—I simply can't physically or mentally function beyond that. Sheer exhaustion and moderate-to-severe pain are issues I am intimately familiar with. However, adding long-haul COVID-19 to that has created a new level of intensity. I'm certain that if I didn't have experience of living with chronic illness, there is no way I would be working with long-haul COVID. Every moment away from patients I spend resting and pacing myself through basic tasks. It's not helping.
Simple actions like showering, brushing my teeth or making food have become monumental tasks. My Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is worse. Minimal activity increases my symptoms which makes it extremely difficult to get back to continuing my neurosurgery recovery—using my recumbent bike, for example. I am beyond frustrated by this.
I continue to have constant lung and chest pain and my sense of smell comes and goes. Headaches and migraine attacks are more frequent and induce a myriad of other symptoms. I am emotionally exhausted and constantly telling others that I am burnt out. I have limited patience at times and am depressed. It is no way to live, but somehow I must forge a path forward.
I have to force myself to get out of bed and go into my home office for patient sessions. I'm too tired to cry, but most mornings I want to weep. Part of me wishes I could just wrap myself in a blanket and do nothing but watch TV and cuddle with my dogs.
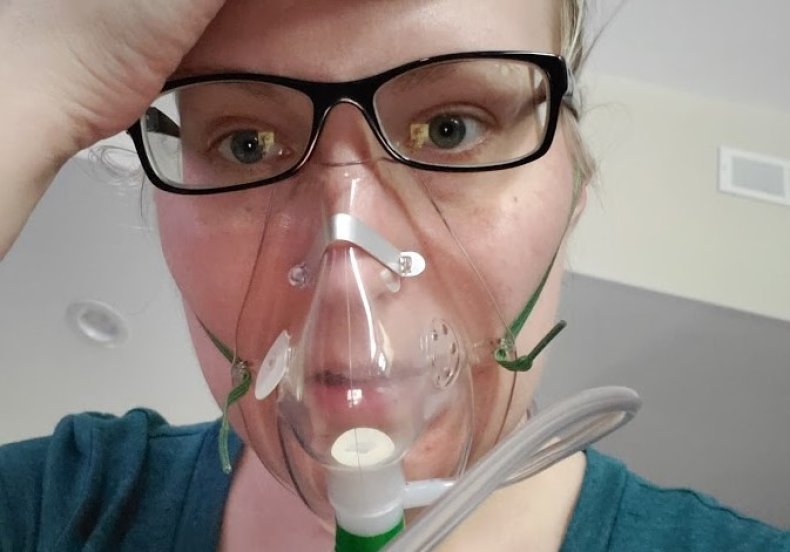
Dr. Melissa Geraghty pictured tackling her COVID-19 symptoms at home in Illinois. Dr. Melissa Geraghty
When people ask how I'm doing, I feel a sense of rising panic—it's exhausting to answer. I suspect people are hoping that I will be "better by now." This is a familiar feeling due to my lived experiences with chronic pain and chronic illness, but it's nevertheless difficult to explain that I am not yet "better."
COVID-19 seems to have taken up permanent residence within my body. There's no telling which symptoms will become more significant or difficult, or if new ones will randomly appear. I don't yet know the extent of damage that has been wrought on my body.
Whether it's from my experiences or those of the many, many others who are living with the ongoing effects of this virus, it's so important for people to understand the gravity of long-haul COVID-19 and how much impact it has. I hope there will be a greater understanding of it as time passes— but this is a virus that doesn't seem to play by the rules.
Dr. Melissa Geraghty, Psy.D. is a Licensed Clinical Health Psychologist. Her clinical focus is on chronic pain, complex medical, and eating disorders. She is an international workshop presenter, a board member, and has received recognition for her advocacy efforts. Dr. Geraghty lives with multiple medical conditions and now long-haul COVID-19. You can follow her on Twitter @MindfulDrG.
All views expressed in this piece are the author's own.
Original Link: https://www.newsweek.com/this-what-its-like-covid-long-hauler-1551431
Don't miss a post!
Sign up today to receive blog posts, program offers, and other occasional emails.
We hate SPAM. We will never sell your information, for any reason.

